From Aging to Cancer: What IGFBP7 Reveals About Women’s Health
[post_date]

Dr. Hursting is a Professor of Nutrition at the UNC Nutrition Research Institute in Kannapolis, NC. He is also Professor in the Department of Nutrition and the Lineberger Comprehensive Cancer Center at the University of North Carolina at Chapel Hill. An international leader in the area of nutrition, obesity, metabolism and cancer, his lab focuses on the molecular and metabolic mechanisms underlying obesity-cancer associations, and the impact of obesity- energy balance modulation (eg, calorie restriction and exercise) or pharmacologic agents on cancer development, progression, and responses to chemotherapy.
What if a simple blood test could reveal who is more likely to face cancer or early death years before symptoms appear? New research led by Stephen Hursting, PhD, MPH, a UNC-Chapel Hill Professor of Nutrition, and then-doctoral student Melissa Orenduff, PhD, suggests that one protein circulating in the blood may do just that.
In a study published this summer in Cancer Epidemiology, Biomarkers & Prevention, the research team identified a blood-based biomarker—insulin-like growth factor–binding protein 7 (IGFBP7)—that was consistently linked with age, obesity, and risk of both cancer and premature death in postmenopausal women. The study followed 793 participants in the Women’s Health Initiative Observational Study for nearly 20 years, making it one of the clearest long-term views we have of how this biomarker relates to women’s health.
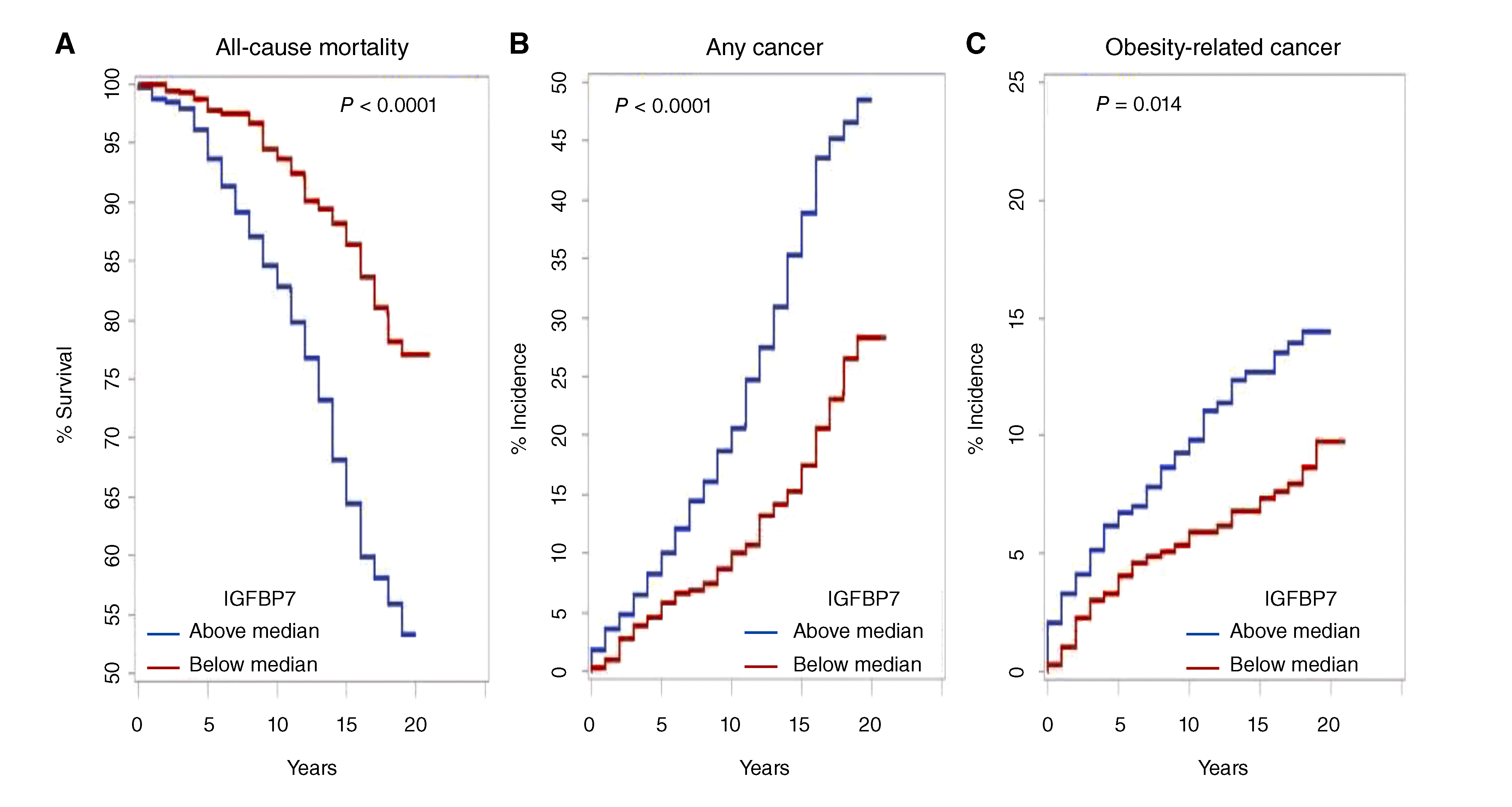
The findings are striking. Women with higher circulating levels of IGFBP7, or a higher ratio of it to IGF-1 – another hormone in the same growth-factor system, faced significantly greater risks of dying or developing cancer during the follow-up period. The effect was strongest for obesity-related cancers, reinforcing the urgent link between excess body weight and cancer vulnerability. Notably, these patterns held even after accounting for lifestyle, socioeconomic, and medical factors, pointing to this biomarker as a robust signal of risk.
Understanding how this biomarker functions helps explain why it may be so powerful. Unlike other proteins in its family, this one interacts not only with growth factors but also with insulin itself, influencing a broad network of biological pathways that are tied to aging, inflammation, and immune regulation. Until now, it had been studied mainly in relation to cardiovascular and kidney disease. This is the first large, longitudinal study showing its potential as a cancer-related biomarker.
“Our findings suggest that IGFBP7 could serve as an early warning signal; an age- and obesity-sensitive biomarker that identifies women at greater risk of developing cancer or dying prematurely,” said Hursting. “This opens the door to new opportunities for prevention and early intervention.”
The data from the Women’s Health Initiative gave the team a rare opportunity to look across nearly two decades of women’s lives. The fact that levels of this protein measured early on could predict outcomes so far into the future underscores its potential value in public health.
As with all discoveries at the NRI, these findings are a beginning, not an end. Future research will need to confirm this biomarker’s role across diverse populations and determine whether targeting this pathway could lead to new prevention strategies. But the promise is clear: a simple blood test could one day help identify individuals most in need of proactive cancer prevention or other health interventions.
At the UNC Nutrition Research Institute, we are committed to advancing precision nutrition and cancer prevention by uncovering the molecular markers that link diet, obesity, and aging to disease. The work of Hursting and Orenduff reminds us that the signals are there, waiting to be read, and that with science and persistence, we can turn those signals into opportunities for healthier, longer lives.
Read the abstract here. Full text may require additional access.
Orenduff MC, Pieper CF, Allott EH, Coleman MF, Jung SY, Vitolins MZ, Fenton JI, Chen C, Kroenke CH, Tabung FK, Barac A, Paskett ED, Pollak MN, Hays-Grudo J, Chang S, Hursting SD. Plasma Insulin-like Growth Factor-Binding Protein-7 Is Positively Associated with Age, Obesity, Mortality, and Cancer in Postmenopausal Women. Cancer Epidemiol Biomarkers Prev. 2025 Jun 3;34(6):922-932. doi: 10.1158/1055-9965.EPI-24-1644. PMID: 40152978.
Dig Deeper
💡Insulin-like growth factors (IGFs) are hormone-like proteins that play a key role in how our bodies grow, repair, and maintain cells. They work alongside insulin to regulate energy use, cell division, and tissue repair.
The IGF system includes IGF-1 and several binding proteins (IGFBPs) that control the amount of IGF that is active in the body. Too much or too little IGF signaling can disrupt this balance – affecting aging, metabolism, and cancer risk.
IGFBP7, the focus of this study, is unusual because it binds only weakly to IGF-1 but interacts with insulin and other pathways that control cell growth, inflammation, and aging. This broader influence makes it a potential regulator of processes that determine disease risk and longevity.
This figure, adapted from the publication referenced in this article, shows survival curves linking IGFBP7 levels to mortality and cancer risk in postmenopausal women.
💡 Figure 2 shows survival curves for women with higher versus lower levels of IGFBP7. The blue line represents women with IGFBP7 above the median, while the red line represents those below. Over nearly 20 years of follow-up, women with higher levels were more likely to die (Panel A) or develop cancer (Panels B and C). These visual gaps between the lines illustrate how IGFBP7, a protein that influences insulin signaling, inflammation, and cellular aging, may serve as an early indicator of health risks tied to age and obesity.