Vitamin D is both a nutrient we eat and a hormone our bodies make when the skin is exposed to sunlight. It is a fat-soluble vitamin that has long been known to help the body absorb and retain calcium and phosphorus; both are critical for building bones. Also, laboratory studies show that vitamin D can reduce cancer cell growth, help control infections, and reduce inflammation. Many of the body’s organs and tissues have receptors for vitamin D, which suggest important roles beyond bone health, and scientists are actively investigating other possible functions.
The daily requirement for vitamin D is at least 15 mcg (600 IU) for women and men under 70 years, and 20 mcg (800 IU) for older people. However, most people are not reaching this requirement. A National Institutes of Health study in 2016 found that the average daily intake of vitamin D from foods and beverages was 5.1 mcg (204 IU) in men and 4.2 mcg (168 IU) in women.
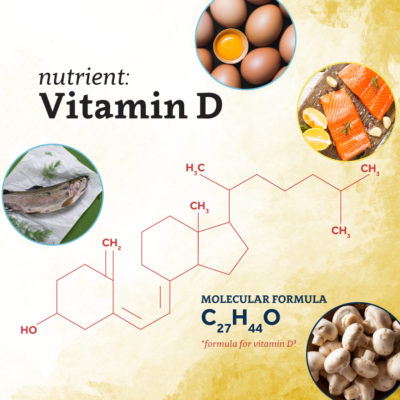
Spending more time in the sun can increase our vitamin D levels, but states above 39°N latitude may find that sun exposure is not enough. Luckily, we can increase our vitamin D intake from foods. Foods with high natural vitamin D concentrations include rainbow trout, salmon, white mushrooms, sardines, egg yolks, and tuna.
Vitamin D deficiency impedes good immune function and has been shown to contribute to seasonal increase of viral respiratory infections, possibly including COVID-19. NRI’s Martin Kohlmeier, MD, PhD, professor of Nutrition, states, “Rigorously remedying vitamin D deficiency, even for a few months during cold and flu seasons, would help reverse known health impacts that include decreased life expectancy and increased mortality. Slowing the spread of COVID-19 would be an important bonus.”
High-risk factors for vitamin D deficiency are:
- Living in northern states1
States below the latitude 39°N saw lower COVID-19 mortality rates in 2020 than states further north. - Dark skin tone2
People with darker skin tone tend to make less vitamin D because skin pigment (melanin) acts like sunscreen, stopping sunlight from making it. - Obesity3
People who are overweight or obese need more vitamin D because much of it gets stuck in belly fat. - Old age3
Older adults tend to get too little vitamin D because their thinner skin makes less of it when sun shines on it and because they spend more time indoors. - Genetic variants4
Common genetic variants strongly lower vitamin D levels. Genetic risk can easily be overcome with enough sunlight and moderately dosed dietary supplements.
Having a combination of high-risk attributes should prompt attention with moderate, individually tailored dose supplementation (usually 4,000 IU or less).
Fortified foods provide most of the vitamin D in American diets. Almost all the US milk supply is voluntarily fortified with about 3 mcg/cup (120 IU), usually in the form of vitamin D33. The United States mandates the fortification of infant formula with 1-2.5mcg/100 kcal (40-100 IU) vitamin D. You can check your food labels to see if the food you’re consuming has been fortified. Foods often fortified include:
- Cheese
- Ice cream
- Soy, almond, or oat milk
- Breakfast cereals
- Orange juice
- Yogurt
- Margarine
Vitamin D can also be taken as a supplement but should only be taken under the care of a physician. Excessive supplement use can lead to toxicity. Vitamin D toxicity is very rare and only due to excessive use of extremely high-dosed supplements. The low amounts of the vitamin we get from food never cause toxicity. Sun exposure cannot lead to toxicity because UV-B light can produce only limited amounts of vitamin D in skin. It is best not to get more than 4,000 IU vitamin D per day from supplements unless on the advice of your doctor.
Sources:
1: https://nutrition.bmj.com/content/bmjnph/3/1/67.full.pdf
2: https://www.hsph.harvard.edu/nutritionsource/vitamin-d/
3: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#h3
4: https://nutrition.bmj.com/content/bmjnph/3/1/106.full.pdf