Microbiome and Nutrition
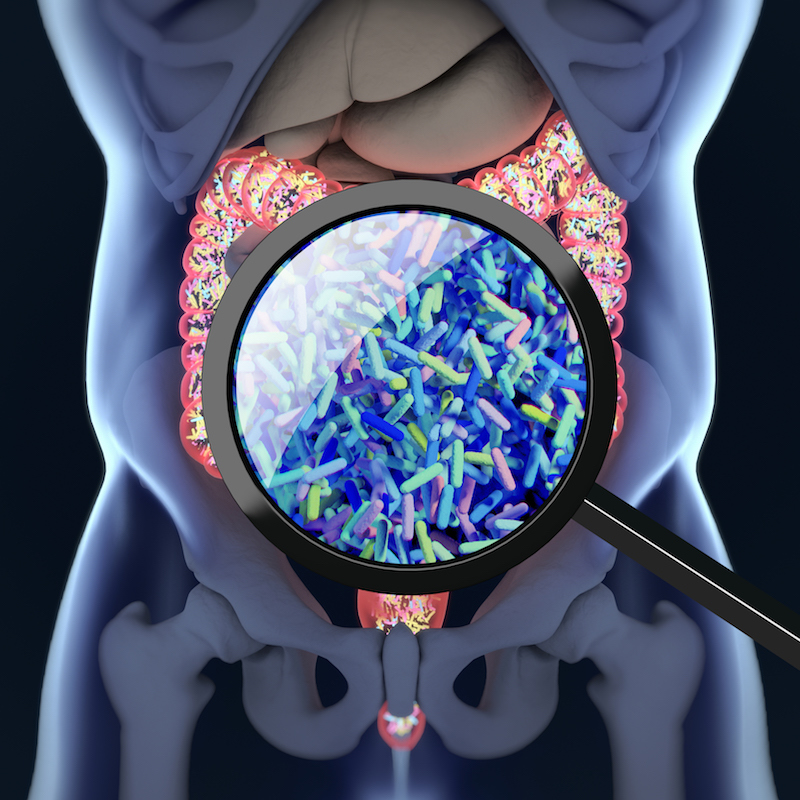
The complex community of bacteria, yeasts and viruses living in our intestines, collectively known as the gut microbiome, is shaped, in part, by what we eat. Genetics, environment, and other factors also influence an individual’s microbial community. Research at the NRI investigates these complex relationships and their impact on disease risk. We use animal models and bioinformatics to study the associations between nutritional metabolites, gut microbiome, and health. What happens in the gut doesn’t stay in the gut. Your microbiome can play a role in cardiovascular disease, obesity and diabetes, and even cancer. Our team envisions a future where analysis of your microbiome can determine disease risk, and medical foods can be prescribed to treat and prevent disease by regulating the microbiome.
Publications
Microbiome and Nutrition Publications
2020
Population studies of TMAO and its precursors may help elucidate mechanisms. Meyer K
2019
Association of dietary patterns with the gut microbiota in older, community-dwelling men. Meyer K
2018
Meta-analysis of human genome-microbiome association studies: the MiBioGen consortium initiative. Meyer K
Human microbiota, blood group antigens, and disease. Sumner S
2017
Trimethylamine N-Oxide, the Microbiome, and Heart and Kidney Disease. Zeisel S
2016
Diet and Gut Microbial Function in Metabolic and Cardiovascular Disease Risk. Meyer K
Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Sumner S
Related News
The immunophilin ligands cyclosporin A and FK506 suppress prostate cancer cell growth by androgen receptor-dependent and -independent mechanisms.
Scavenger receptor class B type I is a plasma membrane cholesterol sensor.
Intestinal SR-BI does not impact cholesterol absorption or transintestinal cholesterol efflux in mice.
Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis.
Susceptibility to diet-induced hepatic steatosis and glucocorticoid resistance in FK506-binding protein 52-deficient mice.
Vitamins and Healthy Diet: A Balancing Act
May 27, 2015 • A vitamin is an organic compound that cannot be made by the human body, but is a required nutrient vital for its various functions. Vitamins are needed in only limited amounts and thus are traditionally derived from our diet. And, yet, nearly half of the U.S. population takes multivitamin supplements—even in times of financial downturn. In 2010 the U.S. supplements industry reached $28 billion in annual sales. And, although no clear scientific need has been defined for vitamin supplementation, the most common reason for taking vitamins is a desire to “improve” or “maintain” overall health, according to a poll conducted by the National Institutes of Health in 2013.